Ultimate Guide To Master 99214 CPT Code
With the advancements in healthcare billing practices, understanding the nuances of CPT codes is vital for doctors to provide accurate documentation and reimbursement. One code that is frequently used in the healthcare and medical industry is the Master 99214 CPT code, which represents an important identifier for evaluation and management services.
Despite its widespread use, CPT Code 99214 might be complicated because of its specific requirements and subtle application details. If you are eager to learn about the Master CPT Code in detail, we have got you covered. In this article, we will explain its significance. We will also discuss the usage of the billing 99214 CPT code. So, without any further ado, here we go!
Table of Contents
- Introduction
- Importance of 99214 CPT Code in Medical Billing
- Documentation Requirements
- Billing and Reimbursement
- How to Use Billing Code 99214 Correctly?
- Recent Updates for 2025
- Determining Eligibility for 99214: Recognizing Suitable Appointments
- Common Mistakes & Challenges in Reporting Code 99214
- Wrapping Up
- Frequently Asked Questions
Introduction
The master 99214 CPT code is a significant identifier in medical billing, especially for management and evaluation services. 99214 CPT code description is generally assigned to office visits, presenting the complexity level and overall intensity that a patient experiences. It means in-depth assessments that call for a complete medical history, a careful examination, and complex medical decision-making.
This code, which specialists and primary care doctors frequently use, represents the complexity of the medical evaluation performed during the visit and the intricate patient contacts. Medical billing practices must comprehend the subtleties of the 99214 CPT code to ensure proper compensation and documentation.
Importance of 99214 CPT Code in Medical Billing
Here are significant reasons why CPT 99214 is essential in HIPAA-compliant telehealth platforms:
1. Correct Representation
99214 CPT Code offers an accurate idea of the duration and complexity of establishing patient encounters. This promotes accurate and fair reimbursement for healthcare via telehealth platforms.
2. Standardized Billing
Standard codes, such as the 99214 CPT Code, lower risk factors and streamline the billing process. Further, it promotes healthcare practice consistency.
3. Reimbursement Determination
Telemedicine app providers can obtain the right payment from payers, including Medicare and commercial insurance, by correctly utilizing code 99214.
Documentation Requirements
To appropriately document a 99214 visit, ensure the following components are addressed:
| Component | Requirements |
|---|---|
| History | – If more than 50% of the encounter is spent on counseling or coordination of care, document the total time spent (typically 30–39 minutes) and the nature of the counseling or coordination activities. |
| Examination | – Detailed Examination: Perform an in-depth assessment of affected body areas or organ systems, typically involving at least six organ systems or a detailed examination of a single organ system. |
| Medical Decision Making (MDM) | – If more than 50% of the encounter is spent on counseling or coordination of care, document the total time spent (typically 30–39 minutes) and the nature of the counseling or coordination activities. |
| Time-Based Coding | – If more than 50% of the encounter is spent on counseling or coordination of care, document the total time spent (typically 30–39 minutes) and the nature of the counseling or coordination activities. |
Proper documentation of these components ensures compliance and supports the medical necessity for billing a 99214 visit. Always tailor documentation to the specific clinical scenario and adhere to the latest coding guidelines.
Read Also: Ultimate Guide to Master 99205 CPT Code in 2025
Billing and Reimbursement
Accurate billing and thorough documentation are essential for ensuring proper reimbursement when using the 99214 CPT code, which denotes a Level 4 evaluation and management (E/M) service for established patients. This level of service typically involves moderate complexity in medical decision-making and requires approximately 25 minutes of face-to-face interaction with the patient.
Reimbursement Rates
As of 2025, the reimbursement rates for CPT code 99214 vary by payer:
- Medicare: The average reimbursement rate is approximately $125.18.
- Medicaid: Reimbursement rates are generally lower than Medicare, averaging around $68.97, though this can vary by state.
- Commercial Insurance: Rates can differ significantly among private insurers. Some payers may reimburse at rates comparable to or higher than Medicare, depending on negotiated contracts and regional factors.
It’s important to note that these figures are averages, and actual reimbursement can vary based on geographic location, payer policies, and specific contractual agreements.
Key Billing Considerations
To optimize reimbursement and minimize the risk of claim denials:
- Documentation: Ensure that the patient’s medical record supports the moderate complexity of medical decision-making required for 99214. This includes detailed notes on the patient’s history, examination findings, and the complexity of medical decisions made during the visit.
- Time-Based Billing: If the visit is predominantly counseling or coordination of care (more than 50% of the encounter), document the total time spent and the nature of the counseling to justify the use of 99214.
- Payer Policies: Stay informed about specific billing requirements and policies of each payer, as they can have unique guidelines for E/M services.
- Modifiers: Apply appropriate modifiers when necessary. For example, Modifier 95 should be used to indicate that a service was provided via telehealth.
Reimbursement Challenges
Common challenges that may affect reimbursement for 99214 include:
- Downcoding: This occurs when the documentation does not adequately support the level of service billed, leading payers to reimburse at a lower rate.
- Denials: This can result from insufficient documentation, lack of medical necessity, or failure to adhere to specific payer guidelines.
- Telehealth Services: With the increasing use of telehealth, it’s crucial to use the correct place of service codes and modifiers to ensure proper reimbursement.
To address these challenges, healthcare providers should:
- Conduct Regular Training: Keep billing and coding staff updated on the latest coding guidelines and payer policies.
- Perform Internal Audits: Regularly review documentation and billing practices to ensure compliance and identify areas for improvement.
- Stay Updated: Monitor changes in the Medicare Physician Fee Schedule (PFS) and updates from private insurers to remain informed about reimbursement trends and policy changes.Centers for Medicare & Medicaid Services
By adhering to these guidelines and maintaining meticulous documentation, healthcare providers can enhance their billing practices for CPT code 99214, leading to improved reimbursement outcomes.
Struggling with 99214 Claims? Fix Them with Automation
Reduce errors, streamline claims, and boost revenue with AI-powered medical billing.
Get a Live DemoHow to Use Billing Code 99214 Correctly?
Here are the key guidelines for accurate usage of billing code 99214:
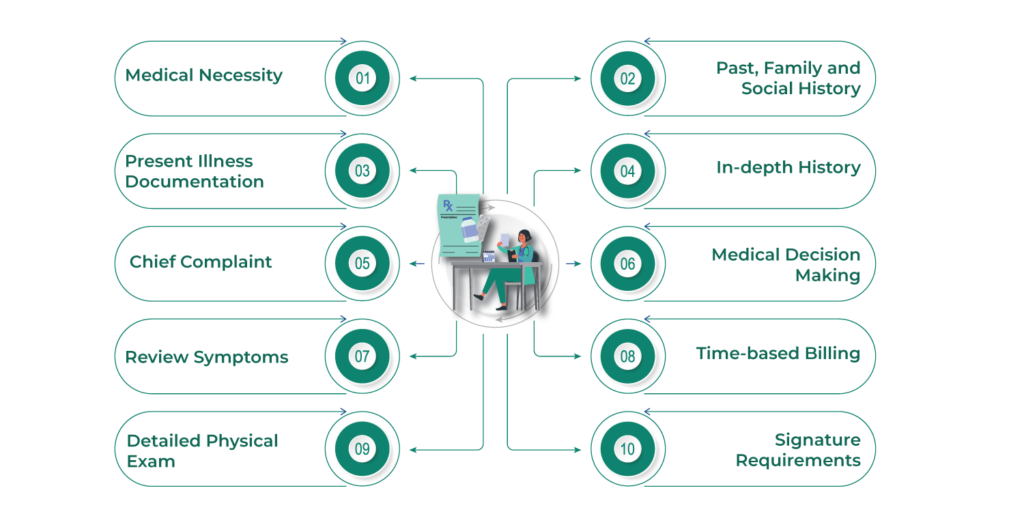
1. Medical Necessity
Procedure code 99214 is used on telehealth apps only when it is necessary to provide healthcare services that meet the specific patient’s requirements. This means there should be a clear reason for the visit, and the care provided should directly address and benefit the patient’s health requirements.
2. Present Illness Documentation
One of the most important things is to record the current condition. You must compile a timeline detailing the evolution of the patient’s current medical condition. The first symptom or indication, or the earlier interaction that led to the current visit, should be the starting point for this documentation.
Provide information about the location, kind, intensity, timing (onset and duration), context of the symptoms, variables modifying the symptoms, and any accompanying signs and symptoms. The aim is to provide a thorough picture of the patient’s state.
3. Chief Complaint
A chief complaint is the patient’s statement highlighting the reason for any medical problem or encounter. It can be anything from a problem, condition, symptoms, diagnosis, or a physician-recommended return visit. Accurate chief complaints are important for excellent evaluation and management of the condition.
4. Review Symptoms
A methodical evaluation of all body systems is conducted by telemedicine software to understand your health fully. Inquire about any symptoms that the patient may have experienced. Record findings like:
- Eyes and Ears
- Nose and Mouth
- Cardiovascular and Respiratory
- Gastrointestinal and Genitourinary
- Musculoskeletal and Integumentary
- Neurologic
5. Detailed Physical Exam
An in-depth physical examination of your body is an essential component, which includes closely examining your organs and affected regions in your body. You must also examine different body symptoms and document these findings in the chest, head, abdomen, neck, genitalia, buttocks, groin, and back.
6. Past, Family and Social History
A thorough examination of the patient’s medical history is the PFSH. It consists of:
- History: The medical history of the patient, including past ailments, surgeries, wounds, and therapies.
- Family history: An examination of medical incidents in the patient’s lineage, encompassing illnesses that could be inherited or carry potential risks.
- Social history: An age-appropriate assessment of previous and ongoing activities that sheds light on lifestyle choices that could impact the patient’s health.
7. In-depth History
A detailed history must include a history of past and present illnesses, the chief complaint, pertinent past family/social history, and an extended review system directly related to the patient’s ongoing healthcare issues via wearable technology in healthcare.
8. Medical Decision Making
When choosing the right E/M code, medical decision-making or MDM is a key factor to consider. For the 99214 CPT Code, a level of “HIGH complexity” MDM is necessary. It includes meeting a minimum of the following two criteria:
- There are many alternatives for diagnosis and therapy management.
- A substantial quantity of information is to be examined.
- There is a high risk of death or morbidity from complications. Consider the “MODERATE complexity” MDM level, which entails a moderate risk of complications or morbidity, and a moderate data review if the “HIGH complexity” 99214 requirements are not satisfied.
9. Time-based Billing
Time will tell if counseling or care coordination takes up more than 50% of the in-person time with the patient. In the patient’s medical file, note the amount of time and the counseling type provided.
10. Signature Requirements
Ensuring that all rendered or ordered services to Medicare beneficiaries are signed appropriately is vital. These signatures can be both electronic and handwritten. Certain documents require stamped signatures.
Your Name. Your Platform. Your Revenue Growth
Launch a fully branded telehealth & billing software with AI-driven automation and seamless integration.
See How It WorksRecent Updates for 2025
In 2025, there are several updates we’ve come across regarding the use of the 99214 CPT Code:
1. Medicare Reimbursement Changes
In 2025, the Medicare conversion factor decreased by approximately 2.83%, from $33.2875 to $32.3465. This reduction affects the reimbursement rates for various services, including CPT code 99214. American Medical Association+1American Medical Association+1
2. Add-On Code G2211
The Centers for Medicare & Medicaid Services (CMS) finalized the implementation of the complexity add-on code G2211. This code can be reported alongside office or outpatient E/M visits, such as those billed under CPT codes 99202-99205 and 99211-99215, including 99214, when additional complexity is involved. This allows for better recognition of the work associated with complex patient care. Centers for Medicare & Medicaid Services
3. Telehealth Services Updates
As of January 1, 2025, new CPT codes (98000-98016) were introduced specifically for telemedicine visits. These codes differentiate between audio-video and audio-only encounters for both new and established patients, effectively replacing the previous telephone-only codes (99441-99443). Healthcare providers should familiarize themselves with these new codes to ensure accurate billing for telehealth services.
4. Documentation Guidelines
The American Medical Association (AMA) provided updated guidelines for Evaluation and Management (E/M) services, emphasizing that the level of service is now determined primarily by medical decision-making (MDM) or total time spent. For CPT code 99214, this includes moderate complexity MDM or a total time of 30-39 minutes spent on the date of the encounter. American Academy of Ophthalmology+1velanhcs.com+1
Healthcare providers should stay informed about these updates to ensure compliance and optimize reimbursement for services rendered under CPT code 99214.
Read Also: An Ultimate Guide To Master 99213 CPT Code
Determining Eligibility for 99214: Recognizing Suitable Appointments
Identifying the eligible visits for a 99214 is a valuable skill. Because identifying suitable appointments for medical code 99214 requires extensive decision-making by reviewing complex medical records, managing moderate to severe conditions qualifies for this CPT code.
Common Mistakes & Challenges in Reporting Code 99214
When it comes to coding, you may experience pros and cons of telemedicine. Some common challenges or mistakes include:
1. Under Coding
Despite its great importance, most healthcare professionals tend to under code, which results in losses. The primary reasons behind this are the chances of abuse or fraud and incomplete documents.
2. Coding Complexity
E/M guidelines are not easy to understand. As a result, every time you try to report code 99214 accurately, it may lead to challenges and mistakes.
3. CPT Coding Changes
Ensuring compliance might be challenging between telehealth vs telemedicine if you don’t stay current with the CPT coding system, which is updated frequently.
Looking for a reliable telemedicine app solution?
Connect with industry-leading developers in the USA.
Get a free consultation today ↗Wrapping Up
Understanding CPT Code 99214 is essential for optimal patient care and accurate billing. It defines the level of service provided and helps optimize reimbursements. By following guidelines and understanding key components, physicians can enhance coding accuracy and maximize reimbursements for office visits.
The Master 99214 CPT code plays a significant role in reimbursement optimization. We hope this article helped you understand the Master 99214 CPT Code in 2025. We discussed the usage of Billing Code 99214 and more in detail. To know more about the 99214 CPT Code, contact experts at VCDoctor, a telemedicine app development company.
Frequently Asked Questions
1. What is the role of medical billing services in ensuring the correct use of CPT codes?
White Label Telemedicine Medical billing services play a significant role in correctly using the CPT code. These include:
- Expertise in medical coding and CPT codes
- Reviewing documentation
- Compliance and regulations
- Coding accuracy
- Revenue maximization
2. How is CPT code 99214 different from 99213?
For quick (15–29 minute) visits with established patients on a virtual doctor app that involve a minimal history, examination, and simple decision-making, use CPT code 99213. A thorough consultation with a thorough history, physical examination, and somewhat complex medical decision-making (30–39 minutes) is denoted by code 99214.
3. What level of care does the 99214 carry?
Code 99214 depicts level-4 care.
4. How to calculate RVU for 99214?
Here is the step-by-step process to calculate RVU for 99214:
- Determine all components, including malpractice, physician work, and practice expense
- Check the updated conversion factor
- Calculate total RVU
- Apply the conversion factor
5. What are some common challenges in documentation and coding?
Some major challenges include:
- Complex and vague coding rules
- Penalties for non-compliance
- Potential for downloading
- Relying on memorization and gut instinct